Overview
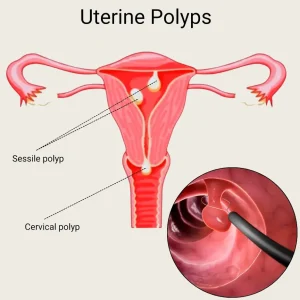
Uterine polyps, also known as endometrial polyps, are growths that develop from the inner lining of the uterus. They are usually noncancerous and vary in size from a few millimeters to several centimeters. Uterine polyps are most common in women between the ages of 40 and 50 but can occur at any age. While many polyps cause no symptoms, some may lead to menstrual irregularities or fertility problems.
Symptoms
Symptoms of uterine polyps depend on their size, number, and location within the uterus.
Common symptoms may include:
-
Irregular menstrual periods
-
Heavy or prolonged menstrual bleeding
-
Bleeding between periods
-
Bleeding after menopause
-
Difficulty getting pregnant or infertility
-
Light spotting or abnormal uterine bleeding
Some women may have uterine polyps without experiencing any noticeable symptoms.
Causes
The exact cause of uterine polyps is not fully understood. Their growth is believed to be influenced by hormonal factors.
Possible causes include:
-
Excess estrogen stimulation of the uterine lining
-
Hormonal imbalances
-
Abnormal response of endometrial tissue to hormones
-
Age-related hormonal changes
Polyps tend to grow during reproductive years and may shrink after menopause.
Risk Factors
Certain factors increase the likelihood of developing uterine polyps.
Risk factors include:
-
Perimenopause or menopause
-
Obesity
-
High blood pressure
-
Use of tamoxifen, a medication used in breast cancer treatment
-
Hormonal disorders affecting estrogen levels
Having risk factors does not necessarily mean polyps will cause symptoms.
Complications
Although uterine polyps are usually benign, they can sometimes lead to complications.
Possible complications include:
-
Infertility or recurrent miscarriage
-
Anemia due to heavy bleeding
-
Recurrence of polyps after treatment
-
Rare risk of cancerous changes, especially after menopause
Early evaluation helps reduce the risk of complications and ensures appropriate management.
Prevention
There is no guaranteed way to prevent uterine polyps, but certain measures may help reduce risk or support early detection.
Preventive steps may include:
-
Maintaining a healthy body weight
-
Managing blood pressure and hormonal conditions
-
Attending regular gynecological checkups
-
Reporting abnormal bleeding promptly
-
Following medical advice when using hormone-related medications
Early diagnosis and treatment improve outcomes and help prevent recurrence or complications.
Advertisement