Overview
Overview
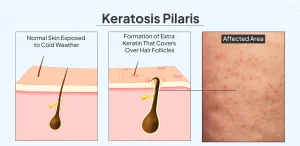
Keratosis pilaris is a common, harmless skin condition that causes small, hard bumps on the skin’s surface. Often referred to as “chicken skin” due to its distinctive appearance, this condition occurs when keratin, a protein that protects skin from infections and harmful substances, builds up and blocks hair follicles. The result is rough patches of tiny bumps that typically appear on the upper arms, thighs, cheeks, and buttocks.
While keratosis pilaris can affect anyone, it most commonly appears during childhood and adolescence. The condition is chronic but generally improves with age, and many people find that their symptoms diminish or disappear entirely by their thirties. Although keratosis pilaris doesn’t pose any health risks and isn’t contagious, many individuals seek treatment for cosmetic reasons or because the affected areas can sometimes feel itchy or irritated.
The bumps associated with keratosis pilaris are usually flesh-colored, white, red, or brown, depending on skin tone. They may become more noticeable in dry weather or when the skin lacks moisture. Understanding this condition can help those affected manage their symptoms and maintain smoother, more comfortable skin.
Symptoms
The hallmark symptom of keratosis pilaris is the appearance of small, painless bumps on the skin. These bumps typically feel rough to the touch and resemble goosebumps or the texture of sandpaper. The bumps are generally the same color as the surrounding skin but can appear pink or red on lighter skin tones and brown or black on darker skin tones.
Common areas where keratosis pilaris appears include the upper arms, front of the thighs, buttocks, and sometimes the face, particularly the cheeks. The bumps usually appear in patches and can vary in number from just a few to hundreds. In some cases, the affected skin may feel dry and rough even when the individual bumps aren’t immediately visible.
Many people with keratosis pilaris experience worsening symptoms during certain times of the year. The condition often becomes more pronounced during winter months when humidity is low and skin tends to be drier. Some individuals may notice slight itching in the affected areas, though significant discomfort is uncommon. The bumps themselves don’t typically cause pain, though they can become irritated if scratched or picked at repeatedly.
Causes
Keratosis pilaris develops when excess keratin accumulates in hair follicles. Keratin is a hard protein found in the outer layer of skin that serves as protection against harmful substances and infection. In people with keratosis pilaris, this protein builds up and forms a plug that blocks the opening of hair follicles, creating the characteristic small bumps.
The exact reason why keratin builds up in some people remains unclear, though researchers believe the condition has a strong genetic component. Many individuals with keratosis pilaris have family members who also experience the condition, suggesting inherited factors play a significant role in its development.
The condition appears to be associated with certain genetic skin disorders and conditions. People with ichthyosis, a group of skin disorders characterized by dry, scaly skin, often develop keratosis pilaris. The link between these conditions suggests that abnormalities in skin cell development and shedding may contribute to keratin buildup.
Environmental factors can also influence the severity of keratosis pilaris symptoms. Dry weather, low humidity, and harsh soaps or skin products can exacerbate the condition by further drying the skin. When skin becomes excessively dry, it can worsen the plugging of hair follicles and make bumps more noticeable.
Risk Factors
Several factors can increase the likelihood of developing keratosis pilaris. Age plays a significant role, with the condition being most common in children and teenagers. While keratosis pilaris can affect people at any age, it typically first appears during early childhood or adolescence and often improves or resolves as people reach adulthood.
Gender may also influence risk, as some studies suggest that keratosis pilaris occurs slightly more frequently in females than in males. However, the condition affects both sexes and can develop in anyone regardless of gender.
Genetic predisposition represents one of the strongest risk factors for keratosis pilaris. Having a family history of the condition significantly increases the chances of developing it. If one or both parents have keratosis pilaris, their children are more likely to experience the condition as well.
Certain skin conditions and health issues can increase susceptibility to keratosis pilaris. People with atopic dermatitis, commonly known as eczema, frequently develop keratosis pilaris alongside their primary skin condition. Those with allergic conditions, including hay fever and asthma, also show higher rates of keratosis pilaris. Additionally, individuals with ichthyosis or other genetic skin disorders that affect the skin’s ability to retain moisture are at elevated risk.
Dry skin conditions, whether genetic or environmental, can contribute to the development or worsening of keratosis pilaris. People living in dry climates or those whose skin naturally produces less oil may be more prone to experiencing symptoms.
Complications
Keratosis pilaris is generally a benign condition that doesn’t lead to serious health complications. The bumps themselves don’t cause pain, don’t indicate an underlying disease, and won’t spread or worsen into more serious skin conditions. Most medical complications associated with keratosis pilaris arise from how people respond to the bumps rather than from the condition itself.
The most common complication occurs when individuals repeatedly scratch, pick, or rub the affected areas. This manipulation can damage the skin, potentially leading to scarring, hyperpigmentation, or areas of darkened skin that persist even after the bumps improve. Breaking the skin barrier through picking can also create openings for bacteria, occasionally resulting in minor infections.
Some people experience temporary changes in skin color where keratosis pilaris bumps were located. After bumps resolve, the affected areas may appear darker or lighter than the surrounding skin for a period of time. This post-inflammatory hyperpigmentation or hypopigmentation typically fades gradually but can be a cosmetic concern for some individuals.
While rare, persistent irritation from clothing friction or aggressive treatment attempts can cause inflammation in the affected areas. This inflammation may make the skin more sensitive and uncomfortable, though it generally resolves when the irritation source is removed.
The psychological and emotional impact of keratosis pilaris can be significant for some people, particularly when bumps appear on visible areas like the arms or face. Concerns about appearance may affect self-confidence and quality of life, especially during adolescence when social pressures are intense. However, it’s important to remember that keratosis pilaris is extremely common and doesn’t reflect poor hygiene or health.
Prevention
While keratosis pilaris cannot be completely prevented, especially in those with genetic predisposition, several strategies can help minimize symptoms and reduce the severity of outbreaks. Maintaining proper skin hydration stands as the most effective approach to managing this condition.
Regular moisturizing helps keep skin supple and reduces the buildup of keratin in hair follicles. Applying thick, emollient moisturizers immediately after bathing, when skin is still slightly damp, helps lock in moisture. Products containing urea, lactic acid, or salicylic acid can be particularly beneficial as they help gently exfoliate the skin and prevent keratin plugs from forming.
Bathing practices significantly influence keratosis pilaris symptoms. Taking short, lukewarm showers or baths instead of long, hot ones helps preserve the skin’s natural oils and prevents excessive drying. Hot water strips away protective oils, potentially worsening symptoms. Using gentle, fragrance-free cleansers rather than harsh soaps maintains the skin’s moisture barrier and reduces irritation.
Gentle exfoliation can help remove excess keratin and prevent follicle blockage. However, aggressive scrubbing should be avoided as it can irritate the skin and worsen inflammation. Using a soft washcloth or gentle exfoliating product two to three times per week is generally sufficient. Over-exfoliation can damage skin and potentially make keratosis pilaris more noticeable.
Protecting skin from dry environmental conditions helps minimize flare-ups. Using a humidifier during dry winter months adds moisture to indoor air, preventing skin from becoming excessively dry. Wearing breathable, soft fabrics that don’t irritate the skin can also reduce friction and inflammation in affected areas.
Avoiding picking or scratching at bumps prevents scarring and skin damage. While the urge to remove bumps manually can be strong, doing so typically worsens the appearance of affected areas and can lead to lasting skin changes. Keeping affected areas well-moisturized often reduces any associated itching, making it easier to leave bumps alone.
Maintaining overall skin health through adequate hydration, balanced nutrition, and protection from excessive sun exposure supports skin function and may help reduce symptom severity. While these measures won’t cure keratosis pilaris, they contribute to healthier skin that’s better able to regulate keratin production and maintain smooth texture.
Advertisement